We think of our brain as the command centre for thoughts, behaviours and actions, but what if we actually had four distinct brains and these functions are the combined result of all four?
Sounds crazy, but this fourth brain is a game changer in how we address neurological illness. To get some context, let’s quickly recap the other three brains…
The first brain
For a long time we thought we controlled ourselves with this one brain inside our head. Over many years this brain was mapped and functions assigned to each area.
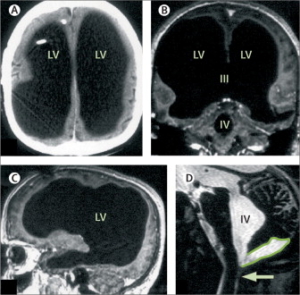
Then an unexpected case in France massively changed our perception of this brain. In 2007, 3 neurologists wrote a paper in a prestigious medical journal called ‘Brain of a white-collar worker’, documenting a 44-year old man who underwent tests for some mild weakness in his leg. To everyone’s absolute astonishment, the CT scan and MRI showed 95% of his brain was missing. As a child he’d had some hydrocephalus (fluid on the brain), but that was simply treated and he continued life without problems. In the images below the white is the bone of the skull, the black is fluid and the thin slice of grey is brain matter. It was always believed we needed this brain tissue to function normally, yet this man was intelligent, married, a father of two and functioning perfectly well on just 5% cerebral mass.[1]
Figure: Massive ventricular enlargement, in a patient with normal social functioning.
Source: Feuillet L, Dufour H, Pelletier J (2007) Brain of a white-collar worker, Lancet 370: 262. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(07)61127-1/fulltext
The second brain
Neurons and glial cells the same as those in the first brain have also been found embedded in the layers of the gastrointestinal tract. This second brain is also known as the enteric nervous system and works autonomously, making decisions on it’s own. Made of around 500 million neurons, the second brain is smaller than the first brain but still contains five times more than the 100 million neurons in the spinal cord and it’s well distributed along the entire length of the digestive tract. It connects to the first brain via the vagus nerve, but we know that when this vagus nerve is severed the second brain continues to function independently of the first brain.
So, your gut really does have a mind of its own and when these two brains don’t co-operate all kinds of gut chaos and mood imbalances are unleashed. For more on this I’d recommend reading The Second Brain by Michael D. Gershon MD.
The third brain
Now it gets a bit weird. While the first and second brains are human, made of human cells, the third brain is made of microbial cells that communicate with our human brains.[2]
An understanding of our gut microbiome began around 2007. The later realisation that this combined mass of commensal microbes in our gut functioned as a third brain, and that we can manipulate it’s composition, opened a door in how to manipulate mental and emotional wellbeing. The microbial cells of this third brain produce hormones and neurotransmitters identical to their human counterparts and directly stimulate neurons in the second brain and communicate with the first brain via the vagus nerve. They influence mood, behaviour, cognition and memory, which are all functions we’d previously associated exclusively with the brain in our head. We even now have the term ‘microbiome-gut-brain axis’ in the scientific literature.[3][4][5]
To fully appreciate the magnitude of the non-human part of us, first understand that our body contains many more bacterial cells than human cells. But what really matters here are the genes that form our DNA as this is the information that makes us who we are. The NIH Microbiome Project has determined that there are around 8,000,000 microbial genes in our body. Compare this to our 22,000 human genes and you see the potentially huge genetic influence this diverse combined microbial mass has on us.[6]
These microbes even have the power to manipulate one of our most fundamental behaviours – eating. They do this by generating cravings for foods that either support their own fitness or suppress their competitors, and also through inducing dysphoria (feeling miserable) until we eat the foods they need, and we can most likely all relate to those overwhelming urges to eat or drink something despite knowing it’s not in our best interests. Fortunately this influence is bi-directional and when this third brain gets out of balance and works against us, we can manipulate the microbiota, and therefore the genetics of this third brain, through diet using prebiotic and probiotic foods.[7]
‘A growing body of preclinical literature has demonstrated bidirectional signaling between the brain and the gut microbiome, involving multiple neurocrine and endocrine signaling mechanisms. While psychological and physical stressors can affect the composition and metabolic activity of the gut microbiota, experimental changes to the gut microbiome can affect emotional behavior and related brain systems. These findings have resulted in speculation that alterations in the gut microbiome may play a pathophysiological role in human brain diseases, including autism spectrum disorder, anxiety, depression, and chronic pain.’ [8]
Thousands of scientific papers can be found exploring the role of the gut microbiome in psychiatric conditions like anxiety and depression. We even now have the term ‘psychobiotics’ referring to probiotics that rebalance the third brain and restore psychological function.[9] A great demonstration of the powerful behavioural and emotional effects these interventions have is provided by a study on mice fed a diet enriched with a specific probiotic called Mycobacterium vaccae. As a comparison another group of mice were fed the same diet without this probiotic and then they were all given maze tests to complete. The mice that didn’t get the probiotic were anxious, afraid and had difficulty exiting the maze, while those given the probiotic were more courageous, less anxious, good at making decisions and able to exit the maze swiftly.[10] That was just one strain, imagine the effects that thousands of strains have in combination. And just to be clear, this particular probiotic is for mice not humans.
The fourth brain
So here we are at the fourth brain, which is also non-human and is the most recent discovery. The term ‘brain microbiome’ was first mentioned in the scientific literature in November 2016 by Dr Marco Ruggiero, who made the connection between two recent paradigm-changing discoveries – the presence of microbes in human brains in 2013 and the discovery of a lymphatic system in the brain in 2015. This is a game-changer in our understanding of the development and persistence of neurological diseases.[11]
To understand how this all fits together lets first look at these two important discoveries.
Microbes in the brain
In 2013, a team of Canadian researchers studied the brains of people who died of HIV/AIDS, believing that opportunistic infections would be found in those brains due to the immune suppressing disease. A control group was needed, which consisted of brains from people who died of different causes who were otherwise immunologically competent. It was always believed that a healthy brain was sterile and microbe-free, but to the amazement of all, the research team found specific microbe populations in ALL the brains studied. They further discovered these brain microbes had immense effects on the brain and only existed in humans and other non-human primates. They were not found in the brains of dogs, cats or other species looked at.[12] When a term like ‘immense’ is used in scientific papers that’s a big deal!
These brain microbes were less diverse than those in the gut, showing a more selective composition with the most abundant type being alpha-Proteobacteria. Interestingly, although these brain microbes were also represented in the gut, many of the abundant gut microbes were not common in the brain, as an example, Firmicutes are one of the most dominant groups in other organs but undetectable in most brains. These microbes were carried into the brain by our immune cells, particularly activated lymphocytes and macrophages, and as our immune cells work in our best interests it’s likely these microbes are beneficial to our brain health and suggests that the acquisition of the Proteobacteria may represent a beneficial organ-specific adaptation.[12]
In fact it may be more remarkable that that even. The bacteria in our brain may have been the trigger for our superior intellect as a species. Of the genes thought to be involved in human evolution, one called RUNX2 is particularly interesting as it may have been responsible for the increase in cranial capacity.[13] What is really unique about this gene is that it’s regulated by probiotics, like those found in fermented foods, which were the first processed foods humans consumed. The RUNX2 gene in apes was different to that in humans and wasn’t able to be stimulated by probiotics. Could it be that the explosive growth in the human brain was down to eating fermented foods? An additional piece of this puzzle is found in an obscure 2013 study that found the RUNX2 gene was positively regulated by Lactobacillus rhamnosus.[14]
Another notable fact about the RUNX2 gene that was responsible for the evolution of the human brain, is that it’s been found to be involved in the development of autism, so it will be interesting to see how the research develops in this area.[15]
Discovery of the brain’s lymphatic system
In 2015 it was discovered that the brain has a lymphatic system and immune cells carried microbes to and from the brain through these lymphatic vessels, which connect into the deep cervical lymph nodes in the neck.[16]
It has also been discovered that when we sleep the brain shrinks slightly to allow the drainage of metabolites from the brain. In layman’s terms that means that our brain cells create waste products which accumulate while we are awake and then when we sleep the cleaners come in to wash them away. As we sleep the brain shrinks to allow more space for this cleansing to take place. This means that a lack of sleep leads to accumulation of toxins in the brain, similar to not emptying the bins in your house, and over time this leads to inflammation that can block the lymph flowing in and out of our brains.[17]
New factors to consider in restoring brain health
When we want to get probiotics to the gut we take them orally or use suppositories. Getting the beneficial microbes into the brain requires different thinking. We know that these microbes are carried to the brain by macrophages, which are cells of our immune system. Waldeyer’s tonsillar ring is a ring of lymphoid tissue inside the mouth and throat containing macrophages that go everywhere in the body including the brain. Each time we swallow the food goes exactly where these macrophages are, so contact with fermented foods in the mouth allows these macrophages to selectively pick up microbes needed by the fourth brain. It seems likely based on this mechanism that swallowing encapsulated probiotics wouldn’t be as effective as eating fermented foods, and eating slowly to prolong interaction in this area could possibly enhance the benefits.
Even if we have the correct microbes present and the macrophages fired up to carry them, we still need a clear road for them to travel. When there are infections in the sinuses, throat and mouth these lymph nodes get clogged and the highway between the third and fourth brains is cut off. This is the really key point in trying to balance the fourth brain – ensuring these vessels are flowing. Chronically inflamed tissue in the nose and throat clogs the cervical nodes where this lymph drains from the brain and so toxic metabolites being cleansed from the brain get trapped in the head along with an accumulate of lymphatic fluid. As the brain is a closed system confined within the skull it can’t expand like other areas of the body do when there’s fluid retention. The inability to drain lymph prevents further uptake of new microbe-enriched lymph and this excess fluid also disrupts connections between neurons. As the immune cells depend on the flow of lymph the immune system of the brain takes a hit leading to an imbalance of brain microbes and chronic inflammation of the brain. These processes are the hallmark of many neurological illnesses. Autism is one of the neurological conditions where this chronic neuroinflammation and excess fluid is commonly observed in the brain.[18]
Another potential problem is infection of the teeth and jaw. Microbes can get trapped in confined spaces within cavities and cavitations (holes in the jaw – usually at tooth extraction sites) and produce unending toxic waste products that inflame and clog this whole lymphatic system. The proximity of the jaw to the cervical lymph nodes in the neck makes this a potentially huge unrecognised issue in brain health.
Summary
So we have at least four brains, all closely integrated but structurally distinct. Two of these brains are non-human and their influence on the human counterparts is immense. We’ve known for some time that the microbiome in the gut affects the brain via the vagus nerve and have tried to rebalance this by taking probiotics. Now, we know why probiotics are so important for brain function, because probiotics ARE cells of the brain, they are inside the brain as the fourth brain and we also need to fix this brain microbiome in addition to the gut one.
While the brain microbiome is partly dependent on a healthy gut microbiome, there are now additional factors to consider. The immune system that connects the four brains is important to transport the microbes into the brain. Healthy macrophages in particular are required and these also need to be effectively activated (read about GcMAF for more on this). Additionally the flow of lymph through the brain’s lymphatic system needs to be working properly by considering chronic infections in the nose, throat and mouth.
How to reconstitute a dysbiotic brain microbiome is complex and a new area being researched – there will be a second blog on this. But what we can already see is that a diet including fermented foods would be beneficial, that those foods should be eaten slowly to encourage maximum interaction with the tonsillar tissue in the mouth, good quality sleep is needed to ensure cleansing of the toxic metabolites that build up in the brain during the day, and attention to infections in the mouth, throat and jaw area. By addressing these areas as well as the specific brain probiotics themselves, we can hopefully expect improvements in brain-related health disorders.
References
- Feuillet L, Dufour H, Pelletier J (2007) Brain of a white-collar worker, Lancet 370: 262. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(07)61127-1/fulltext
- Greenlaw P and Ruggiero M (2015) Your Third Brain: The Revolutionary New Discovery to Achieve Optimum Health.
- Carabotti et al (2015) The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 28: 203–209. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/
- Cryan and O’Mahony (2011) The microbiome-gut-brain axis: from bowel to behavior. Neurogastroenterol Motil. 23(3):187-92. https://www.ncbi.nlm.nih.gov/pubmed/21303428
- Forsythe P1, Kunze WA. (2013) Voices from within: gut microbes and the CNS. Cell Mol Life Sci. 70:55-69. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.462.3838&rep=rep1&type=pdf
- NIH Human Microbiome Project defines normal bacterial makeup of the body: Genome sequencing creates first reference data for microbes living with healthy adults. https://www.nih.gov/news-events/news-releases/nih-human-microbiome-project-defines-normal-bacterial-makeup-body
- Alcock J et al (2014) Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. Bioessays. 36:940-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4270213/
- Mayer et al (2014) Gut Microbes and the Brain: Paradigm Shift in Neuroscience. J Neurosci. 34(46): 15490–15496. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4228144/
- Sarkar A et al (2016) Psychobiotics and the Manipulation of Bacteria-Gut-Brain Signals. Trends Neurosci. 39:763-781. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5102282/
- Matthews DM, Jenks SM (2013) Ingestion of Mycobacterium vaccae decreases anxiety-related behavior and improves learning in mice. Behav Processes. 96:27-35. https://www.ncbi.nlm.nih.gov/pubmed/23454729
- Ruggiero M (2016) Fecal Microbiota Transplantation and the Brain Microbiota in Neurological Diseases. Clin Endosc. 49(6): 579. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5152774/
- Branton WG et al. (2013) Brain microbial populations in HIV/AIDS: α-proteobacteria predominate independent of host immune status. PLoS One. 8:e54673 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3552853/
- Magherini S, et al (2015) Metopic suture and RUNX2, a key transcription factor in osseous morphogenesis with possible important implications for human brain evolution. Ital J Anat Embryol. 120:5-20. https://www.ncbi.nlm.nih.gov/pubmed/26738254
- Maradonna F et al (2013) Probiotic Supplementation Promotes Calcification in Danio rerio Larvae: A Molecular Study. PLoS One. 8:e83155. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3866187/
- Benítez-Burraco A, Murphy E (2016) The Oscillopathic Nature of Language Deficits in Autism: From Genes to Language Evolution. Front Hum Neurosci. 10:120. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4796018/
- Louveau A (2015) Structural and functional features of central nervous system lymphatic vessels. Nature. 523:337-41. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4506234/
- Xie L et al (2013) Science. 2013 Oct 18;342(6156):373-7. Sleep drives metabolite clearance from the adult brain. Science. 342:373-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3880190/
- Bradstreet JJ, Ruggiero M, Pacini S (2015) Commentary: Structural and functional features of central nervous system lymphatic vessels. Front Neurosci. 9:485. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4686591/

Leave A Comment